Approaches to Population Health Measurement
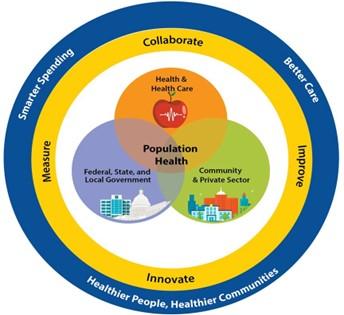
The population health of a group is dependent upon the interplay of several factors (e.g., economic, social, environmental, cultural, behavioral), of which clinical care represents only a portion (Stoto, 2014). As such, population health depends on a multiplicity of factors, many of which are not within CMS’s traditional role to address as a health care services payor. Because of this, the achievement of measurement and improvement in population health depends upon innovation, collaboration, and coordination across interested parties. These include local, tribal, state, national government agencies, and the community, such as members of the care team, payors, hospitals, and nursing homes in delivering care to the target population(s), as well as community members and organizations. The Population Health and the Triple Aim figure reflects this overlap of roles in improving population health and showing the joint influence on population health outcomes by health care, government, the community, and the private sector.
Population health improvement requires a multisector approach. Government agencies, including tribal agencies, measured entities and payors, community service providers, and the private sector can join to improve the health of every person and population in their communities, together through measurement, innovation, collaboration, and improvement to achieve the triple aim goals of better care, smarter spending, and healthier people and communities.
No single entity in the public or private sector has sole capacity or responsibility for overall population health improvement. Multiple organizations, public and private, perform public health activities. As opposed to other sectors with interorganizational partnerships and alliances, these public health activities are largely uncoordinated, leading to gaps, inefficiencies, and gaps in care (Deprez & Thomas, 2016; Mays & Scutckfield, 2010). Systems thinking—understanding the collective effect of multiple actors and actions—is necessary to organize and sustain population health improvement (Woulfe et al., 2010). There must be “a shared measurement system.” By extension, a multi-sector approach is essential to addressing the multiple determinants of population health. Emerging partnerships between measured entities, federal, state, tribal, local health agencies, community service providers, multiple other organizations (e.g., education systems and the justice system), and the private sector can help call attention to underlying problems, shift resources to increase returns on investments, and sustain population-level improvements in health. Stoto (2014) noted measurement is critical to improving population health. The Institute of Medicine (IOM), now known as the National Academy of Medicine (NAM), said “Without a strong measurement capability, the nation cannot learn what initiatives and programs work best, resources cannot be guided toward the most promising strategies, and there is little ability to promote accountability in results” (IOM, 2013a, p. 2).
Parrish (2010) identified three approaches to measuring population health:
- aggregating health outcome measurements made on people into summary statistics, such as population averages or medians
- assessing the distribution of individual health outcome measures in a population and among specific population subgroups
- measuring the function and well-being of the population or society itself, as opposed to individuals
In 2013, the IOM, identified criteria for selecting and prioritizing measures of quality for use in population health improvement:
Conditions or outcomes for measurement should be
- reflective of a high preventable burden
- actionable at the appropriate level for intervention
Measures should be
- timely
- usable for assessing various populations
- understandable
- methodologically rigorous
- accepted and harmonized
Of particular importance is CMS’ partnerships with state agencies, Medicaid in particular. States are in the best position to assess the unique needs of their respective Medicaid-eligible populations and drive reforms that result in better health outcomes. CMS is committed to ushering in a new era for the federal and state Medicaid partnership, where states have more freedom to design programs meeting the spectrum of diverse needs of their Medicaid population. CMS aims to empower all states to advance the next wave of innovative solutions to Medicaid’s challenges – solutions focusing on improving quality, accessibility, and outcomes in the most cost- effective manner. This approach is supported by findings from the Medicaid and CHIP Payment and Access Commission (MACPAC), which highlights the critical role states play in shaping population health strategies tailored to their Medicaid populations and emphasizes the importance of cross-sector collaboration to address social determinants of health (MACPAC, 2014). Working together, through local organizations, tribal agencies, state agencies, other parts of HHS (e.g., Indian Health Service), and federal partners such as the Departments of Education, Agriculture, Transportation, Housing and Urban Development, and Veterans’ Affairs, CMS believes they can collectively manage and improve population health for all individuals and families served by CMS programs.
Current CMS initiatives seeking to focus on improving population health and not focusing solely on the quality of care rendered by a singular measured entity include
- Accountable Care Organizations (ACOs): ACOs are responsible for clinical care, costs, and outcomes in a particular population of Medicare patients.
- Accountable Health Communities (AHCs) Model: AHCs address a gap between clinical care and community services in the health care delivery system by testing whether identifying and addressing the health-related social needs of Medicare and Medicaid beneficiaries through screening, referral, and community navigation services will impact health care costs and reduce health care utilization.
- Medicare Advantage plans (MA plans): MA plans are responsible for care in the population of enrollees. MA plans may provide additional services not covered by traditional Medicare (Long et al., 2022), such as transportation to appointments and non-permanent home modifications to allow beneficiaries to age in place.
- Program of All-Inclusive Care for the Elderly (PACE): PACE is a Medicare and Medicaid program that provides comprehensive medical and social services to certain frail, elderly people living in the community. PACE helps people meet their health care and social needs in the community instead of going to a nursing home or other care facility.
- Medicaid Health Homes: The Health Home program, established under the Affordable Care Act, supports states in coordinating care for Medicaid beneficiaries with chronic conditions, focusing on whole-person care and population health management.
- Delivery System Reform Incentive Payment (DSRIP) Programs: DSRIP programs provide states with funding to support projects that improve care delivery, population health, and cost-effectiveness in Medicaid.